Continuous Glucose Monitors (CGMs) are medical devices that track blood glucose levels in real-time, providing continuous data to patients and healthcare providers. These devices measure glucose concentrations in interstitial fluid through a small sensor inserted under the skin, eliminating the need for frequent fingerstick blood tests. CGMs display glucose readings at regular intervals, typically every one to five minutes, and can store data for extended periods to reveal glucose patterns and trends.
This continuous monitoring capability allows for more precise insulin dosing and timing, improved meal planning, and better overall diabetes management strategies.
The global prevalence of diabetes has increased substantially in recent decades. The International Diabetes Federation reported that approximately 537 million adults worldwide had diabetes in 2021, with projections indicating continued growth in the coming years. This rising prevalence has created greater demand for effective glucose monitoring technologies.
CGMs have demonstrated clinical benefits including improved glycemic control, reduced frequency of severe hypoglycemic episodes, and enhanced quality of life for many users. Research indicates that CGM use can lead to lower hemoglobin A1C levels and decreased time spent in dangerous glucose ranges, potentially reducing the risk of long-term diabetic complications.
Key Takeaways
- Continuous Glucose Monitors (CGMs) provide real-time glucose readings through a sensor placed under the skin.
- CGMs offer significant benefits, including better glucose control and reduced need for finger-prick tests.
- Compared to traditional methods, CGMs deliver continuous data, enabling more informed diabetes management decisions.
- Despite their advantages, CGMs face challenges such as sensor accuracy, cost, and user comfort.
- Future advancements aim to improve CGM technology, enhancing diabetes care and patient quality of life.
How Continuous Glucose Monitors Work
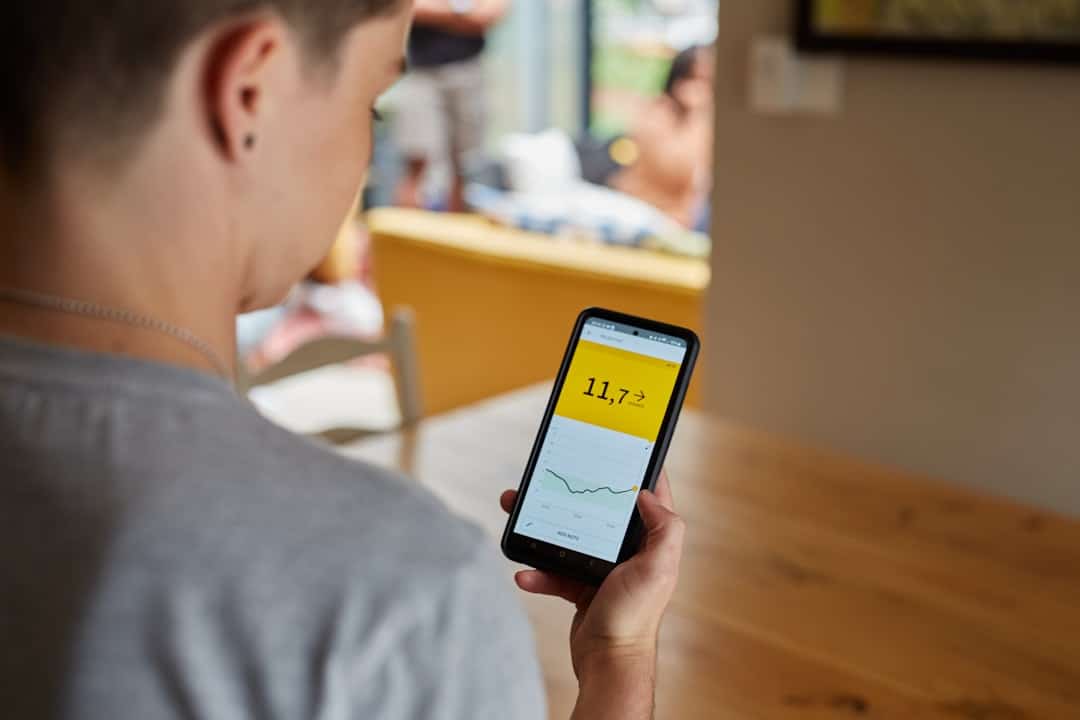
Continuous Glucose Monitors operate through a sophisticated system that involves a small sensor placed under the skin, typically on the abdomen or arm. This sensor measures glucose levels in the interstitial fluid, which is the fluid surrounding cells in the body. The data collected by the sensor is transmitted wirelessly to a receiver or smartphone app, where users can view their glucose levels in real-time.
Most CGMs provide readings every few minutes, allowing for continuous tracking of glucose trends rather than isolated snapshots. The technology behind CGMs relies on electrochemical sensors that detect glucose concentrations. When glucose molecules interact with the sensor, they produce an electrical signal proportional to the glucose level.
This signal is then converted into a readable format and displayed on the user’s device. Many modern CGMs also feature alarms that alert users when their glucose levels are too high or too low, providing an additional layer of safety. Some devices even integrate with insulin pumps, allowing for automated insulin delivery based on real-time glucose readings, further enhancing diabetes management.
Benefits of Continuous Glucose Monitoring

The benefits of Continuous Glucose Monitoring are manifold and extend beyond mere convenience. One of the most significant advantages is the ability to identify patterns and trends in glucose levels over time. This continuous data stream enables users to recognize how various factors—such as food intake, physical activity, stress, and sleep—affect their blood sugar levels.
By understanding these relationships, individuals can make more informed choices about their lifestyle and treatment plans. Moreover, CGMs can significantly reduce the frequency of hypoglycemic episodes, which are dangerously low blood sugar levels that can lead to serious health complications. With real-time alerts and trend data, users can take proactive measures to prevent hypoglycemia before it occurs.
Studies have shown that individuals using CGMs experience fewer severe hypoglycemic events compared to those relying solely on traditional monitoring methods. Additionally, CGMs can enhance overall glycemic control, as evidenced by improvements in HbA1c levels among users. This long-term measure of blood sugar control is crucial for reducing the risk of diabetes-related complications such as neuropathy, retinopathy, and cardiovascular disease.
Comparison with Traditional Glucose Monitoring Methods
When comparing Continuous Glucose Monitors to traditional glucose monitoring methods, such as fingerstick blood tests, several key differences emerge. Traditional methods typically involve pricking a finger to obtain a blood sample, which is then analyzed using a glucometer. This process provides a snapshot of blood glucose levels at a specific moment but does not account for fluctuations that may occur between tests.
As a result, individuals may miss critical information about their glucose trends and patterns. In contrast, CGMs provide a continuous stream of data that captures fluctuations in glucose levels throughout the day and night. This comprehensive view allows users to see how their glucose levels respond to various stimuli in real-time.
While traditional methods may require multiple fingersticks throughout the day—often leading to discomfort and inconvenience—CGMs offer a more user-friendly approach with minimal disruption to daily life. Furthermore, many CGMs allow for data sharing with healthcare providers, enabling more collaborative and informed decision-making regarding treatment adjustments.
Impact on Diabetes Management
| Metric | Before CGM | After CGM | Impact |
|---|---|---|---|
| Frequency of Glucose Monitoring | 4-6 times per day (finger pricks) | Continuous, every 5 minutes | Increased data points for better glucose management |
| Hypoglycemia Detection | Often missed or detected late | Real-time alerts for low glucose levels | Reduced risk of severe hypoglycemia |
| Average HbA1c Reduction | 7.5% (typical baseline) | 6.8% (with CGM use) | Improved long-term glucose control |
| Time in Range (70-180 mg/dL) | 50-60% | 70-75% | Better glucose stability |
| Patient Quality of Life | Moderate, due to finger pricks and uncertainty | Improved, less finger pricks and more confidence | Enhanced daily diabetes management experience |
| Emergency Room Visits for Diabetes | Higher frequency due to hypo/hyperglycemia | Reduced frequency | Lower healthcare burden |
The impact of Continuous Glucose Monitoring on diabetes management is profound and multifaceted. For many users, CGMs have transformed their approach to managing diabetes from reactive to proactive. With access to real-time data, individuals can make immediate adjustments to their diet or insulin regimen based on their current glucose levels.
This capability is particularly beneficial during periods of physical activity or illness when glucose levels may fluctuate unpredictably. Additionally, CGMs have been shown to improve patient engagement and adherence to treatment plans. The ability to visualize glucose trends empowers users to take ownership of their health and fosters a greater understanding of how lifestyle choices affect their condition.
Research indicates that patients who use CGMs are more likely to adhere to recommended dietary guidelines and exercise regimens compared to those who rely solely on traditional monitoring methods. This increased engagement can lead to better overall health outcomes and a higher quality of life for individuals living with diabetes.
Challenges and Limitations of Continuous Glucose Monitors

Despite their numerous advantages, Continuous Glucose Monitors are not without challenges and limitations. One significant concern is the cost associated with these devices. While prices have decreased over time, CGMs can still be expensive, particularly for those without insurance coverage or with high deductibles.
The financial burden may deter some individuals from utilizing this technology, limiting access to those who could benefit most from continuous monitoring. Another challenge lies in the accuracy of CGM readings. Although advancements in technology have improved accuracy significantly, discrepancies can still occur between interstitial fluid measurements and actual blood glucose levels.
Factors such as dehydration or sensor placement can affect readings, leading to potential misinterpretations of glucose status. Users must remain vigilant and continue to perform occasional fingerstick tests to confirm CGM readings when necessary. Additionally, some individuals may experience skin irritation or allergic reactions at the sensor site, which can further complicate consistent use.
Future Developments in Continuous Glucose Monitoring Technology
The future of Continuous Glucose Monitoring technology holds great promise as researchers and developers continue to innovate in this field. One area of focus is improving sensor accuracy and reliability through advanced materials and algorithms that enhance data interpretation. For instance, next-generation sensors may utilize nanotechnology or biocompatible materials that minimize discomfort while providing more precise readings.
Another exciting development is the integration of artificial intelligence (AI) into CGM systems. AI algorithms can analyze vast amounts of data collected from users to identify patterns and predict future glucose trends more accurately. This predictive capability could lead to personalized recommendations for insulin dosing or dietary adjustments based on individual responses over time.
Furthermore, advancements in connectivity may enable seamless integration with other health devices and platforms, creating a comprehensive ecosystem for diabetes management that includes wearables, mobile apps, and telehealth services.
The Role of Continuous Glucose Monitors in Improving Diabetes Care
Continuous Glucose Monitors represent a significant advancement in diabetes care, offering patients unprecedented access to real-time data about their glucose levels. By facilitating proactive management strategies and enhancing patient engagement, CGMs have transformed how individuals approach their diabetes treatment plans. While challenges remain regarding cost and accuracy, ongoing innovations promise to address these issues and expand access to this vital technology.
As diabetes continues to affect millions worldwide, the role of Continuous Glucose Monitors will only become more critical in improving health outcomes and quality of life for those living with this chronic condition. The integration of advanced technologies such as AI and improved sensor designs will further enhance the capabilities of CGMs, making them an indispensable tool in modern diabetes management strategies.
Continuous glucose monitors (CGMs) are revolutionizing diabetes management by providing real-time data that empowers patients to make informed decisions about their health. For those interested in technology that enhances daily life, you might find it useful to read about how to choose the right iPhone for you in 2023, as smartphones can play a crucial role in managing health apps and tracking glucose levels. Check out the article here for more insights.
FAQs
What is a Continuous Glucose Monitor (CGM)?
A Continuous Glucose Monitor (CGM) is a medical device that continuously measures glucose levels in the interstitial fluid just beneath the skin. It provides real-time glucose readings throughout the day and night, helping individuals with diabetes manage their blood sugar levels more effectively.
How does a Continuous Glucose Monitor work?
A CGM uses a small sensor inserted under the skin to detect glucose levels in the interstitial fluid. The sensor sends data to a receiver or smartphone app, which displays glucose readings and trends. This allows users to monitor their glucose levels continuously without frequent fingerstick tests.
Why are Continuous Glucose Monitors important for diabetes management?
CGMs provide real-time glucose data, enabling users to detect high and low blood sugar levels promptly. This helps in making informed decisions about diet, exercise, and medication, reducing the risk of complications and improving overall diabetes control.
Who can benefit from using a Continuous Glucose Monitor?
People with type 1 diabetes, type 2 diabetes, and those who require intensive insulin therapy can benefit from CGMs. They are especially useful for individuals who experience frequent hypoglycemia or have difficulty maintaining stable glucose levels.
Are Continuous Glucose Monitors accurate?
Modern CGMs are highly accurate and have been approved by regulatory agencies like the FDA. However, they may have slight delays compared to blood glucose meters, as they measure glucose in interstitial fluid rather than directly in the blood.
Do Continuous Glucose Monitors replace fingerstick blood glucose tests?
While CGMs reduce the need for frequent fingerstick tests, users may still need to perform occasional fingerstick tests to calibrate the device or confirm readings during rapid glucose changes.
What are the benefits of using a Continuous Glucose Monitor?
Benefits include improved glucose control, reduced hypoglycemia episodes, better understanding of glucose trends, increased convenience, and enhanced quality of life for people with diabetes.
Are there any limitations or challenges with Continuous Glucose Monitors?
Limitations include the cost of devices and sensors, the need for sensor replacement every few days to weeks, potential skin irritation at the insertion site, and the requirement for user training to interpret data effectively.
How has the use of Continuous Glucose Monitors changed diabetes management?
CGMs have transformed diabetes care by providing continuous, real-time glucose data, enabling proactive management, reducing complications, and supporting personalized treatment plans. They have also facilitated remote monitoring and telehealth services.
Can Continuous Glucose Monitors be used with insulin pumps?
Yes, many CGMs can be integrated with insulin pumps to create automated insulin delivery systems, also known as artificial pancreas systems, which adjust insulin doses based on glucose readings for better glucose control.