Digital health records, often referred to as electronic health records (EHRs), represent a transformative shift in the way patient information is stored, accessed, and managed within the healthcare system. Unlike traditional paper-based records, EHRs facilitate the digital collection and sharing of patient data, enabling healthcare providers to deliver more efficient and coordinated care. The transition to digital records has been driven by advancements in technology, the need for improved patient outcomes, and the demand for streamlined administrative processes.
As of 2023, a significant majority of healthcare facilities in developed countries have adopted EHR systems, reflecting a growing recognition of their potential benefits. The implementation of digital health records has not only enhanced the accessibility of patient information but has also improved the accuracy and completeness of medical histories. With EHRs, healthcare providers can quickly retrieve critical information such as allergies, medications, and past treatments, which is essential for making informed clinical decisions.
Furthermore, EHRs can integrate data from various sources, including laboratories and imaging centers, creating a comprehensive view of a patient’s health status. This interconnectedness fosters better communication among healthcare teams and ultimately leads to improved patient care.
Key Takeaways
- Digital health records are electronic versions of a patient’s medical history, treatment plans, and other health-related information.
- Privacy in digital health records is crucial for maintaining patient confidentiality and trust in the healthcare system.
- Legal and ethical considerations play a significant role in the collection, storage, and sharing of digital health records.
- Security measures such as encryption, access controls, and regular audits are essential for protecting digital health records from unauthorized access and breaches.
- Patients should have access to and control over their health information, including the ability to review, update, and share their records as they see fit.
Importance of Privacy in Digital Health Records
The Trust Between Patients and Healthcare Providers
Patients entrust their healthcare providers with highly personal information, including medical histories, treatment plans, and even genetic data. This trust is predicated on the assurance that their information will be kept confidential and secure. When privacy is compromised, it can lead to significant emotional distress for patients and undermine their willingness to seek care or disclose vital information.
The Consequences of Privacy Breaches
Moreover, the implications of privacy breaches extend beyond individual patients; they can have far-reaching consequences for healthcare organizations as well. A breach can result in substantial financial penalties, damage to reputation, and loss of patient trust. For instance, the Health Insurance Portability and Accountability Act (HIPAA) in the United States imposes strict regulations on how patient information must be handled and protected.
Maintaining Privacy: An Ethical Obligation and Operational Necessity
Non-compliance can lead to hefty fines and legal repercussions for healthcare providers. Therefore, maintaining privacy is not only an ethical obligation but also a critical component of operational integrity within healthcare organizations.
Legal and Ethical Considerations
The legal landscape surrounding digital health records is complex and multifaceted. Various laws and regulations govern the collection, storage, and sharing of health information to protect patient privacy. In the United States, HIPAA sets forth national standards for the protection of health information, mandating that healthcare providers implement safeguards to ensure confidentiality.
Additionally, state laws may impose further restrictions or requirements regarding patient data protection. For example, some states have enacted laws that grant patients greater control over their health information or require explicit consent before sharing data with third parties. Ethically, healthcare providers face the challenge of balancing patient autonomy with the need for data sharing in clinical practice.
Patients have a right to control their own health information; however, this autonomy must be weighed against the benefits of sharing data for treatment coordination and public health initiatives. Ethical frameworks such as beneficence (acting in the best interest of patients) and non-maleficence (avoiding harm) guide healthcare professionals in navigating these dilemmas. The ethical obligation to protect patient privacy must be upheld while also recognizing that data sharing can lead to improved health outcomes through research and population health management.
Security Measures for Protecting Digital Health Records
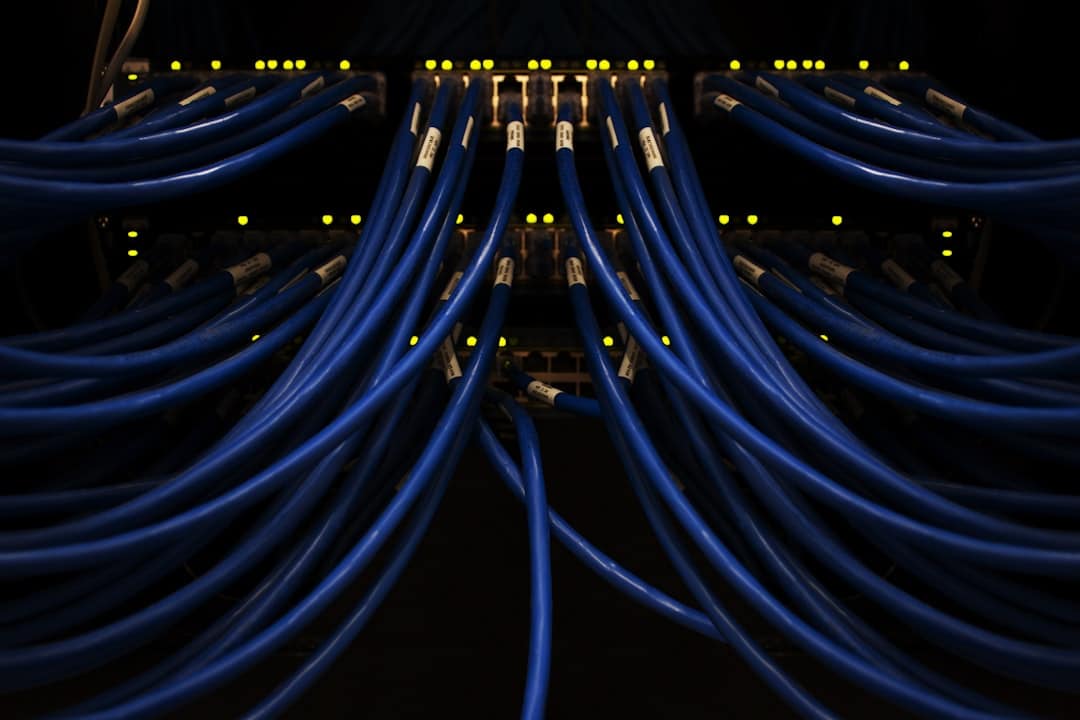
To safeguard digital health records from unauthorized access and breaches, healthcare organizations must implement robust security measures. These measures encompass both technical solutions and administrative protocols designed to protect sensitive information. One fundamental aspect of security is encryption, which transforms data into a coded format that can only be accessed by authorized users with the appropriate decryption keys.
Encryption is particularly crucial when transmitting health information over networks or storing it on cloud-based platforms. In addition to encryption, access controls play a vital role in protecting digital health records. Organizations should employ role-based access controls (RBAC) that limit access to sensitive information based on an individual’s job responsibilities.
For instance, a nurse may have access to a patient’s medication history but not to their billing information. Regular audits and monitoring of access logs can help identify any unauthorized attempts to access data, allowing organizations to respond swiftly to potential threats. Furthermore, ongoing staff training on cybersecurity best practices is essential to ensure that employees are aware of potential risks and understand their role in maintaining data security.
Patient Access and Control over Their Health Information
Empowering patients with access to their own health information is a critical aspect of modern healthcare delivery. Digital health records facilitate this access by allowing patients to view their medical histories, test results, and treatment plans through secure online portals. This transparency not only enhances patient engagement but also fosters a sense of ownership over one’s health journey.
Patients who are informed about their medical conditions are more likely to participate actively in their care decisions and adhere to treatment recommendations. Moreover, patients should have control over how their health information is shared with third parties. Many EHR systems now include features that allow patients to grant or revoke consent for data sharing with specific providers or organizations.
This capability aligns with the principles of patient autonomy and informed consent, ensuring that individuals have a say in who accesses their sensitive information. However, it is essential for healthcare organizations to educate patients about their rights regarding data access and sharing so that they can make informed choices about their health information.
Potential Risks of Privacy Breaches in Digital Health Records
Identity Theft and Financial Fraud
One of the most immediate consequences of a privacy breach is the potential for identity theft. When unauthorized individuals gain access to personal health information, they may use it to commit fraud or impersonate patients for financial gain.
Stigmatization and Discrimination
Beyond identity theft, privacy breaches can lead to stigmatization and discrimination against patients. Sensitive information related to mental health conditions, substance abuse histories, or genetic predispositions can be misused if it falls into the wrong hands. For example, if an employer gains access to an employee’s mental health records without consent, it could result in discrimination in hiring or promotion decisions.
Psychological Impact and Barriers to Care
The psychological impact on patients who fear exposure of their private information can deter them from seeking necessary medical care or disclosing critical details to their providers.
Balancing Privacy with Data Sharing for Research and Public Health
While protecting patient privacy is paramount, there is also a compelling need for data sharing in research and public health initiatives. The aggregation of health data can lead to significant advancements in medical research, epidemiology, and public health policy development. For instance, during public health crises such as pandemics, timely access to aggregated health data can inform decision-making processes and resource allocation strategies.
To strike a balance between privacy and data sharing, researchers and public health officials must adhere to ethical guidelines that prioritize patient confidentiality while allowing for necessary data utilization. De-identification techniques can be employed to remove personally identifiable information from datasets used for research purposes. This approach enables researchers to analyze trends and outcomes without compromising individual privacy.
Additionally, obtaining informed consent from patients before using their data for research purposes fosters transparency and trust between patients and researchers.
Future Trends in Privacy and Digital Health Records
As technology continues to evolve, so too will the landscape of digital health records and privacy considerations. One emerging trend is the integration of artificial intelligence (AI) into EHR systems. AI has the potential to enhance data analysis capabilities while also improving security measures through advanced threat detection algorithms.
However, the use of AI raises new ethical questions regarding data ownership and algorithmic bias that must be addressed as these technologies become more prevalent. Another trend is the increasing emphasis on patient-centric models of care that prioritize transparency and control over personal health information. As patients become more aware of their rights regarding data privacy, they will demand greater involvement in decisions about how their information is used.
This shift may lead to the development of new technologies that empower patients with tools for managing their own health data securely. In conclusion, while digital health records offer numerous advantages for improving patient care and operational efficiency within healthcare systems, they also present significant challenges related to privacy protection. As we move forward into an increasingly digital future, it will be essential for stakeholders across the healthcare spectrum—providers, policymakers, researchers, and patients—to collaborate in developing solutions that uphold privacy while harnessing the power of data for better health outcomes.
In a recent article on enicomp.com, the importance of privacy in managing digital health records was discussed in depth.
For more information on the latest trends in technology, check out this article on the top trends on TikTok in 2023.
FAQs
What is the role of privacy in managing digital health records?
Privacy plays a crucial role in managing digital health records as it ensures that sensitive personal health information is protected from unauthorized access, use, and disclosure.
Why is privacy important in digital health records management?
Privacy is important in digital health records management to maintain patient confidentiality, trust, and security of sensitive health information. It also helps to comply with privacy laws and regulations.
How is privacy maintained in managing digital health records?
Privacy in managing digital health records is maintained through the use of encryption, secure access controls, regular audits, and compliance with privacy regulations such as HIPAA and GDPR.
What are the potential risks of not prioritizing privacy in digital health records management?
Not prioritizing privacy in digital health records management can lead to unauthorized access, data breaches, identity theft, and loss of patient trust. It can also result in legal and financial consequences for healthcare organizations.
What are some best practices for ensuring privacy in managing digital health records?
Best practices for ensuring privacy in managing digital health records include implementing strong data encryption, conducting regular security assessments, providing staff training on privacy protocols, and obtaining patient consent for data sharing.