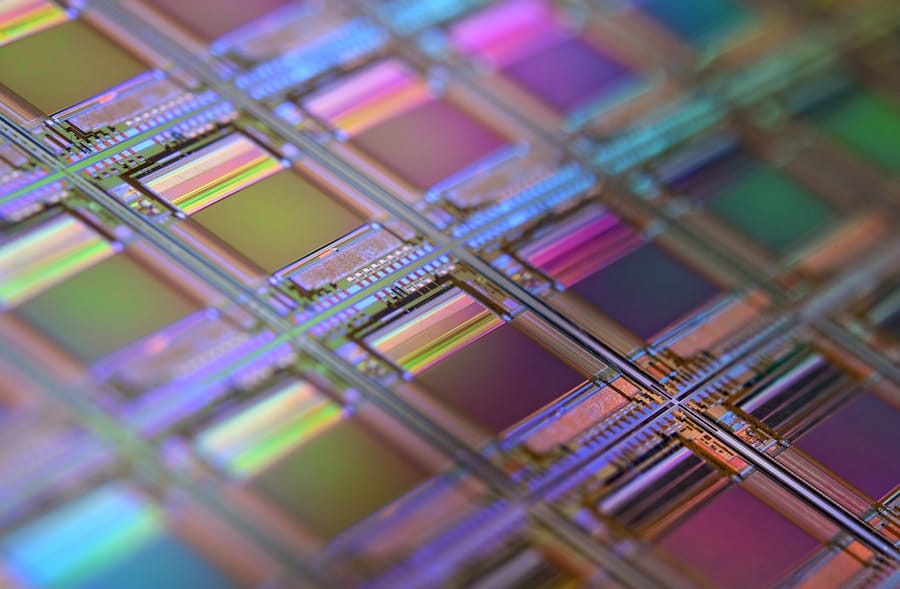
Biochips represent a significant advancement in the field of biotechnology, serving as miniature laboratories that can perform multiple biological analyses simultaneously. These devices, often composed of a small piece of glass or silicon embedded with thousands of microscopic probes, have the capacity to detect and analyze biological markers, such as DNA, RNA, proteins, and other molecules. The integration of biochips into healthcare monitoring systems is paving the way for a new era of personalized medicine, where treatments and health management strategies can be tailored to the individual characteristics of each patient.
This shift from a one-size-fits-all approach to a more customized methodology is not only enhancing the efficacy of treatments but also improving patient outcomes and satisfaction. Personalized healthcare monitoring involves the continuous assessment of an individual’s health status through various means, including wearable devices, mobile applications, and now, biochips. These technologies enable healthcare providers to gather real-time data about a patient’s health, allowing for timely interventions and adjustments to treatment plans.
The synergy between biochips and personalized healthcare monitoring is particularly promising, as it allows for the collection of vast amounts of data that can be analyzed to identify trends, predict health issues, and optimize therapeutic strategies. As we delve deeper into the implications of biochips in healthcare, it becomes evident that they are not merely tools for analysis but are integral components of a broader movement towards precision medicine.
Key Takeaways
- Biochips are small devices that can be used for personalized healthcare monitoring, allowing for real-time analysis of an individual’s health status.
- Biochips revolutionize healthcare monitoring by providing rapid and accurate results, enabling early detection and personalized treatment of diseases.
- Personalized healthcare monitoring is important as it allows for tailored treatment plans based on an individual’s unique genetic makeup and health profile.
- Biochips play a crucial role in disease detection and management by enabling the analysis of biomarkers and genetic information for early diagnosis and targeted therapy.
- The advantages of biochips in personalized healthcare monitoring include rapid results and tailored treatment, but limitations include cost and the need for further research and development.
How Biochips Revolutionize Healthcare Monitoring
The revolution brought about by biochips in healthcare monitoring is multifaceted. One of the most significant contributions is their ability to facilitate high-throughput screening, which allows for the simultaneous analysis of numerous samples. This capability is particularly beneficial in clinical settings where time is of the essence.
For instance, biochips can be employed to screen for genetic mutations associated with various diseases, enabling healthcare providers to identify at-risk patients quickly. This rapid identification can lead to earlier interventions, which are often critical in managing diseases such as cancer or genetic disorders. Moreover, biochips enhance the accuracy and sensitivity of diagnostic tests.
Traditional methods may require multiple steps and extensive sample processing, which can introduce errors and delays. In contrast, biochips streamline these processes by integrating multiple functions onto a single platform. For example, microarray biochips can analyze gene expression levels across thousands of genes simultaneously, providing a comprehensive view of a patient’s genetic profile.
This level of detail not only aids in diagnosis but also informs treatment decisions by identifying which therapies are likely to be most effective based on an individual’s unique genetic makeup.
The Importance of Personalized Healthcare Monitoring
Personalized healthcare monitoring is crucial in today’s medical landscape as it shifts the focus from reactive to proactive care. By continuously tracking an individual’s health metrics, healthcare providers can detect deviations from normal ranges early on, allowing for timely interventions that can prevent the progression of diseases. This proactive approach is particularly vital in managing chronic conditions such as diabetes or hypertension, where regular monitoring can significantly reduce complications and improve quality of life.
Furthermore, personalized healthcare monitoring fosters patient engagement and empowerment.
This engagement can lead to better adherence to treatment plans and lifestyle modifications, as patients are more likely to take ownership of their health when they understand how their behaviors impact their well-being.
For instance, wearable devices that sync with biochip data can provide real-time feedback on physical activity levels or dietary choices, encouraging individuals to make healthier decisions.
The Role of Biochips in Disease Detection and Management
Biochips play a pivotal role in the early detection and management of diseases by providing precise and rapid diagnostic capabilities. In oncology, for example, biochips can be used to detect circulating tumor DNA (ctDNA) in blood samples, allowing for non-invasive cancer screening and monitoring. This method not only reduces the need for invasive biopsies but also enables clinicians to track tumor dynamics over time, adjusting treatment strategies based on real-time data regarding tumor response.
In addition to cancer detection, biochips are instrumental in managing infectious diseases. The COVID-19 pandemic highlighted the need for rapid testing solutions, and biochip technology rose to the occasion by enabling the development of tests that could detect viral RNA within hours. These advancements have implications beyond COVID-19; they can be applied to other infectious diseases such as HIV or hepatitis C, where early detection is crucial for effective treatment and containment strategies.
By integrating biochips into routine screening protocols, healthcare systems can enhance their ability to respond swiftly to emerging health threats.
Advantages and Limitations of Biochips in Personalized Healthcare Monitoring
The advantages of biochips in personalized healthcare monitoring are numerous and impactful. One significant benefit is their ability to provide comprehensive data sets that inform clinical decision-making. By analyzing multiple biomarkers simultaneously, biochips can reveal complex interactions within biological systems that may not be apparent through traditional testing methods.
This holistic view enables healthcare providers to develop more nuanced treatment plans tailored to individual patient needs. However, despite their many advantages, biochips also come with limitations that must be addressed. One primary concern is the potential for false positives or negatives due to variations in sample quality or processing errors.
Such inaccuracies can lead to misdiagnosis or inappropriate treatment decisions, underscoring the need for rigorous validation protocols before biochip technologies are widely adopted in clinical practice. Additionally, the cost associated with developing and implementing biochip technology can be prohibitive for some healthcare systems, particularly in low-resource settings where access to advanced diagnostic tools is limited.
Ethical and Privacy Considerations in Biochip Technology
As with any emerging technology in healthcare, biochips raise important ethical and privacy considerations that must be carefully navigated. The collection and analysis of personal health data through biochips necessitate robust data protection measures to safeguard patient privacy. Concerns about data breaches or unauthorized access to sensitive health information are paramount, especially as biochip technology becomes more integrated into everyday healthcare practices.
Moreover, ethical dilemmas arise regarding informed consent and the potential for genetic discrimination. Patients must be fully informed about how their data will be used and who will have access to it. There is also the risk that genetic information obtained through biochip analysis could be used against individuals by employers or insurance companies, leading to discrimination based on predisposition to certain health conditions.
Addressing these ethical challenges requires a collaborative effort among policymakers, healthcare providers, and technology developers to establish clear guidelines that protect patient rights while promoting innovation in personalized healthcare monitoring.
Future Trends and Developments in Biochips for Personalized Healthcare Monitoring
The future of biochip technology in personalized healthcare monitoring is poised for significant advancements driven by ongoing research and innovation. One promising trend is the integration of artificial intelligence (AI) with biochip analysis. AI algorithms can process vast amounts of data generated by biochips more efficiently than traditional methods, identifying patterns and correlations that may elude human analysts.
This synergy could lead to more accurate predictions regarding disease risk and treatment efficacy. Additionally, miniaturization and portability are key areas of development for biochip technology.
For instance, point-of-care testing devices equipped with biochip technology could enable patients to conduct tests at home or in remote locations, facilitating immediate feedback on their health status without the need for extensive laboratory infrastructure.
The Impact of Biochips on Personalized Healthcare Monitoring
The impact of biochips on personalized healthcare monitoring is profound and far-reaching. By enabling rapid diagnostics and continuous health assessments tailored to individual needs, biochips are transforming how healthcare is delivered and experienced. As technology continues to evolve, the potential for biochips to enhance disease detection, management, and prevention will only grow stronger.
In this dynamic landscape, it is essential for stakeholders across the healthcare spectrum—researchers, clinicians, policymakers—to collaborate in addressing the challenges posed by this technology while harnessing its benefits for improved patient care. The journey towards fully realizing the potential of biochips in personalized healthcare monitoring is just beginning; however, their promise holds great hope for a future where healthcare is more precise, efficient, and accessible than ever before.
For more information on the latest trends in technology, check out the article TheNextWeb brings insights to the world of technology. This article provides valuable insights into the ever-evolving world of technology and how it impacts various industries, including healthcare. Stay informed on the latest developments and innovations that are shaping the future of personalized healthcare monitoring.
FAQs
What is a biochip?
A biochip is a small device that contains a grid of miniaturized test sites, known as microarrays, that can perform multiple tests simultaneously. These tests can include detecting specific DNA sequences, proteins, or other molecules.
How are biochips used in personalized healthcare monitoring?
Biochips are used in personalized healthcare monitoring to analyze a patient’s genetic makeup, detect specific biomarkers, and monitor the effectiveness of treatments. This allows for tailored healthcare interventions based on an individual’s unique genetic and molecular profile.
What are the benefits of using biochips in personalized healthcare monitoring?
The use of biochips in personalized healthcare monitoring allows for early detection of diseases, more accurate diagnosis, and personalized treatment plans. It also enables continuous monitoring of a patient’s health status, leading to better disease management and improved outcomes.
Are there any limitations to using biochips in personalized healthcare monitoring?
Some limitations of using biochips in personalized healthcare monitoring include the need for specialized equipment and expertise, as well as the potential for high costs. Additionally, biochips may have limitations in detecting certain biomarkers or genetic variations.
What are some examples of biochip applications in personalized healthcare monitoring?
Biochips are used in personalized healthcare monitoring for a variety of applications, including cancer screening, pharmacogenomics (tailoring drug treatments based on genetic variations), monitoring of chronic diseases, and early detection of genetic disorders.

