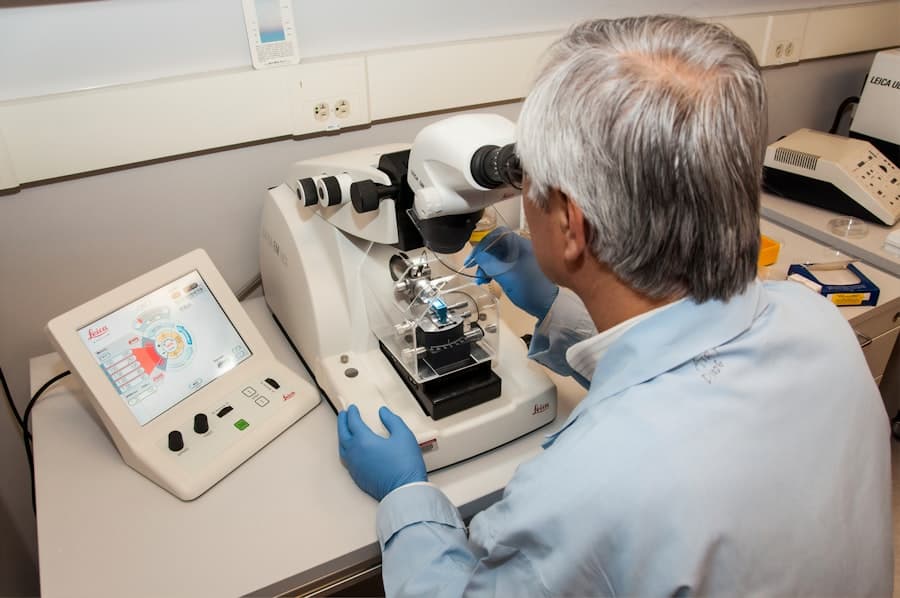
The integration of artificial intelligence (AI) into clinical trials represents a transformative shift in the landscape of medical research. Traditionally, clinical trials have been labor-intensive, requiring extensive human resources and time to gather and analyze data. However, the advent of AI technologies has introduced new methodologies that enhance the efficiency and accuracy of these trials.
By leveraging machine learning algorithms and advanced data analytics, researchers can now process vast amounts of information at unprecedented speeds, leading to more informed decision-making and potentially faster drug development timelines. AI’s role in clinical trials extends beyond mere data analysis; it encompasses patient recruitment, monitoring, and outcome prediction. The ability to analyze electronic health records, genetic information, and real-time patient data allows AI systems to identify suitable candidates for trials more effectively than traditional methods.
This not only accelerates the recruitment process but also ensures that the selected participants are more likely to respond positively to the treatment being tested. As a result, AI is not just a tool for efficiency; it is a catalyst for innovation in how clinical trials are designed and executed.
Key Takeaways
- AI is revolutionizing clinical trials by predicting patient outcomes and improving efficiency.
- Predicting patient outcomes is crucial for identifying the most effective treatments and improving patient care.
- AI utilizes a vast amount of data, including patient history, genetics, and treatment responses, to predict patient outcomes.
- AI has a significant impact on clinical trial efficiency by streamlining processes and reducing time and costs.
- Ethical considerations in AI predictions include privacy, bias, and the need for human oversight in decision-making.
The Importance of Predicting Patient Outcomes
Predicting patient outcomes is a critical component of clinical trials, as it directly influences the success of new therapies and interventions. Accurate predictions can help researchers understand how different patient populations will respond to treatments, which is essential for tailoring therapies to individual needs. This personalized approach not only enhances the likelihood of successful outcomes but also minimizes the risk of adverse effects, thereby improving patient safety and satisfaction.
Moreover, the ability to predict outcomes can significantly impact the overall design of clinical trials. For instance, if researchers can identify specific biomarkers or genetic profiles associated with positive responses to a treatment, they can design trials that focus on these populations. This targeted approach not only increases the chances of success but also optimizes resource allocation by reducing the number of participants who may not benefit from the intervention.
In essence, predicting patient outcomes is not merely an academic exercise; it is a fundamental aspect of developing effective and safe medical therapies.
How AI Utilizes Data to Predict Patient Outcomes

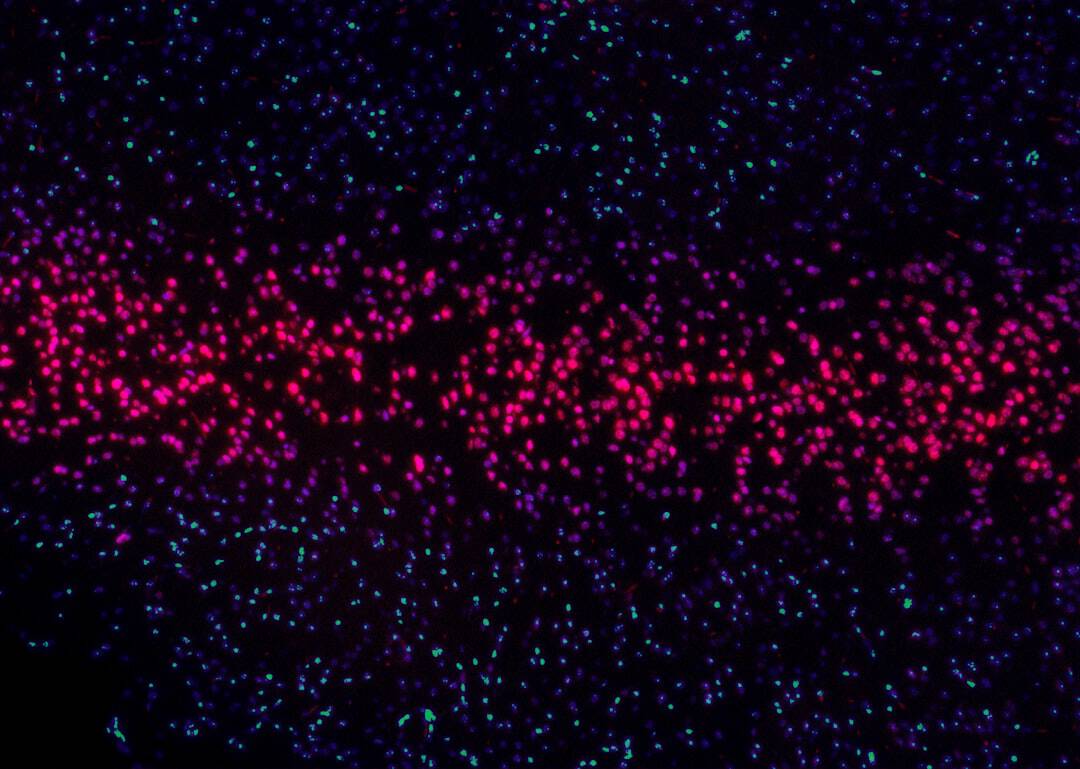
AI employs sophisticated algorithms to analyze diverse datasets, extracting meaningful patterns that can inform predictions about patient outcomes. One of the primary methods used is machine learning, which allows AI systems to learn from historical data and improve their predictive capabilities over time. For example, by training on datasets that include patient demographics, medical histories, treatment regimens, and outcomes, AI can develop models that predict how new patients with similar profiles might respond to a given treatment.
In addition to structured data, AI can also process unstructured data sources such as clinical notes, imaging studies, and genomic sequences. Natural language processing (NLP) techniques enable AI systems to interpret and analyze text-based information from electronic health records, extracting relevant insights that contribute to outcome predictions. This multifaceted approach allows for a more comprehensive understanding of patient health and treatment responses, ultimately leading to more accurate predictions.
The Impact of AI on Clinical Trial Efficiency
The incorporation of AI into clinical trials has led to significant improvements in efficiency across various stages of the research process. One of the most notable impacts is on patient recruitment. Traditional recruitment methods often involve lengthy processes that can delay trial initiation.
However, AI-driven algorithms can quickly sift through large databases of potential participants, identifying those who meet specific criteria based on their medical history and current health status. This rapid identification not only accelerates recruitment but also enhances the diversity of trial populations, which is crucial for ensuring that findings are generalizable across different demographics. Furthermore, AI enhances monitoring during clinical trials by enabling real-time data analysis.
This proactive approach can lead to timely adjustments in treatment protocols or even early termination of trials if necessary. By streamlining these processes, AI contributes to a more agile research environment where decisions can be made based on real-time insights rather than relying solely on periodic assessments.
Ethical Considerations in AI Predictions
While the benefits of AI in clinical trials are substantial, they also raise important ethical considerations that must be addressed. One major concern is the potential for bias in AI algorithms. If the training data used to develop predictive models is not representative of the broader population, there is a risk that the predictions will favor certain groups over others.
This could lead to disparities in treatment access and outcomes, undermining the principle of equity in healthcare. Additionally, the use of AI in predicting patient outcomes raises questions about informed consent and data privacy. Patients must be adequately informed about how their data will be used and the implications of AI-driven predictions on their treatment options.
Ensuring transparency in how AI systems operate and make decisions is essential for maintaining trust between patients and researchers. As AI continues to evolve within clinical trials, it is imperative that ethical frameworks are established to guide its implementation and address these concerns.
Challenges and Limitations of AI in Predicting Patient Outcomes
Despite its potential, the application of AI in predicting patient outcomes is not without challenges and limitations. One significant hurdle is the quality and availability of data. For AI algorithms to function effectively, they require large volumes of high-quality data that accurately reflect patient populations and treatment responses.
However, many healthcare systems struggle with fragmented data sources and inconsistent data entry practices, which can hinder the development of robust predictive models. Moreover, there is a risk that reliance on AI predictions may lead to overconfidence in automated decision-making processes. While AI can provide valuable insights, it should not replace clinical judgment or human expertise.
The complexity of human health and disease often requires nuanced understanding that goes beyond what algorithms can offer. Therefore, integrating AI into clinical practice necessitates a balanced approach that combines technological advancements with human oversight.
Future Implications of AI in Clinical Trial Predictions
Looking ahead, the future implications of AI in clinical trial predictions are vast and promising. As technology continues to advance, we can expect even more sophisticated algorithms capable of integrating diverse data sources seamlessly. The potential for real-time analytics will allow researchers to adapt trial protocols dynamically based on ongoing results, leading to more responsive and effective research methodologies.
Furthermore, as personalized medicine gains traction, AI will play an increasingly vital role in tailoring treatments to individual patients based on their unique genetic makeup and health profiles. This shift towards precision medicine will not only enhance treatment efficacy but also reduce costs associated with ineffective therapies. The ongoing collaboration between data scientists, clinicians, and regulatory bodies will be crucial in shaping a future where AI-driven predictions become standard practice in clinical trials.
The Role of AI in Shaping the Future of Clinical Trials
The integration of artificial intelligence into clinical trials marks a significant evolution in how medical research is conducted. By enhancing our ability to predict patient outcomes and streamline trial processes, AI holds the potential to revolutionize drug development and improve patient care. However, as we embrace these advancements, it is essential to remain vigilant about ethical considerations and challenges that accompany this technology.
As we move forward into an era where AI becomes increasingly embedded in clinical research, its role will undoubtedly expand beyond mere prediction into areas such as real-time monitoring and adaptive trial designs. The collaboration between technology and human expertise will be paramount in ensuring that these innovations lead to equitable healthcare solutions that benefit all patients. The future of clinical trials is poised for transformation, with AI at the forefront driving progress toward more effective therapies and improved health outcomes for diverse populations worldwide.