Predictive genomics is an emerging field that leverages genetic information to forecast an individual’s risk of developing certain diseases or health conditions. By analyzing a person’s genome, researchers can identify genetic variants that may predispose them to various health issues, ranging from common ailments like diabetes and heart disease to rare genetic disorders. This innovative approach not only enhances our understanding of the genetic underpinnings of diseases but also paves the way for more proactive healthcare strategies.
The integration of predictive genomics into clinical practice represents a paradigm shift, moving from reactive treatment models to preventive care that emphasizes early intervention and personalized health management. The foundation of predictive genomics lies in the vast amount of data generated by advancements in sequencing technologies. The Human Genome Project, completed in 2003, was a monumental milestone that provided a comprehensive map of human DNSince then, the cost of sequencing has plummeted, making it feasible for researchers and clinicians to analyze genomes at an unprecedented scale.
As a result, predictive genomics has gained traction in both research and clinical settings, offering insights that were previously unattainable. The potential applications of this field are vast, encompassing not only disease prediction but also the development of tailored treatment plans based on an individual’s unique genetic makeup.
Key Takeaways
- Predictive genomics uses genetic information to predict an individual’s risk of developing certain diseases or conditions.
- Predictive genomics plays a crucial role in preventive healthcare by enabling early detection and intervention for at-risk individuals.
- Advancements in predictive genomics technology, such as genome sequencing and bioinformatics, have improved the accuracy and accessibility of genetic testing.
- Ethical considerations in predictive genomics include privacy concerns, potential discrimination, and the need for informed consent.
- Predictive genomics has a significant impact on personalized medicine by guiding treatment decisions based on an individual’s genetic makeup.
The Role of Predictive Genomics in Preventive Healthcare
Early Detection and Intervention
By identifying high-risk individuals, healthcare providers can implement targeted screening programs and lifestyle modifications. For instance, individuals with a family history of breast cancer may undergo genetic testing for BRCA1 and BRCA2 mutations, which significantly increase the risk of developing the disease. If a mutation is identified, proactive measures such as increased surveillance or prophylactic surgeries can be considered, ultimately reducing morbidity and mortality associated with breast cancer.
Personalized Lifestyle Recommendations
Predictive genomics can also inform personalized lifestyle recommendations that align with an individual’s genetic predispositions. For example, individuals with a genetic predisposition to cardiovascular disease may benefit from tailored dietary advice, exercise regimens, and stress management techniques designed to lower their risk factors.
Empowering Patients and Improving Health Outcomes
This personalized approach not only empowers patients to take charge of their health but also fosters a collaborative relationship between patients and healthcare providers. By integrating genetic insights into preventive care, the healthcare system can shift its focus from treating diseases to preventing them, leading to improved health outcomes and reduced healthcare costs.
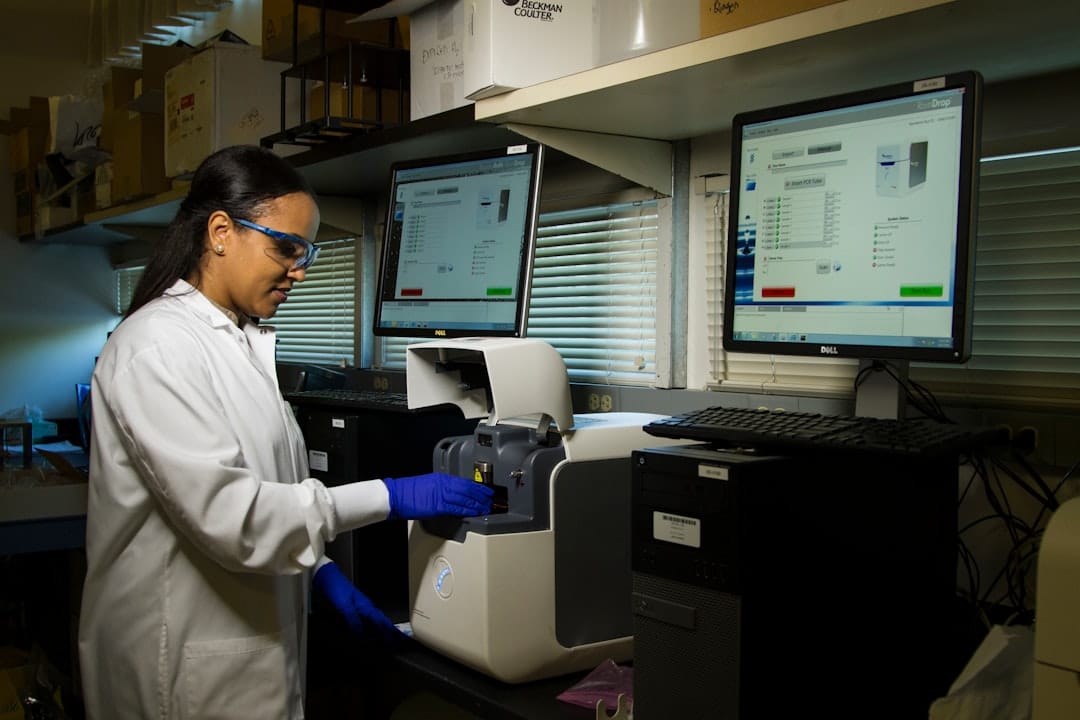
Advancements in Predictive Genomics Technology

The rapid advancements in genomic technologies have significantly propelled the field of predictive genomics forward. Next-generation sequencing (NGS) has revolutionized the ability to sequence entire genomes quickly and affordably. This technology allows for the simultaneous analysis of millions of DNA fragments, providing comprehensive insights into an individual’s genetic makeup.
As a result, researchers can identify not only single nucleotide polymorphisms (SNPs) associated with disease risk but also larger structural variations that may contribute to complex health conditions. In addition to NGS, bioinformatics tools have become increasingly sophisticated, enabling researchers to analyze vast datasets and extract meaningful patterns from genomic information. Machine learning algorithms are now being employed to predict disease risk based on genetic data, integrating various factors such as environmental influences and lifestyle choices.
These advancements have led to the development of polygenic risk scores (PRS), which aggregate the effects of multiple genetic variants to provide a more nuanced assessment of an individual’s risk for certain diseases. As these technologies continue to evolve, they hold the promise of enhancing our ability to predict health outcomes with greater accuracy and precision.
Ethical Considerations in Predictive Genomics
As predictive genomics continues to advance, it raises important ethical considerations that must be addressed to ensure responsible use of genetic information. One major concern is the potential for genetic discrimination, where individuals may face adverse consequences in employment or insurance based on their genetic predispositions. The Genetic Information Nondiscrimination Act (GINA) was enacted in the United States to protect individuals from such discrimination; however, gaps remain in coverage and enforcement.
Ensuring that individuals feel safe sharing their genetic information is paramount for the success of predictive genomics in clinical practice. Informed consent is another critical ethical issue in predictive genomics. Patients must fully understand the implications of genetic testing, including potential psychological impacts and the possibility of discovering unexpected results.
Genetic counseling plays a vital role in this process, helping individuals navigate the complexities of their genetic information and make informed decisions about testing and subsequent actions. Additionally, there are concerns regarding data privacy and security; as genomic data becomes increasingly integrated into electronic health records, safeguarding this sensitive information from breaches is essential to maintain public trust in predictive genomics.
The Impact of Predictive Genomics on Personalized Medicine
Predictive genomics is fundamentally transforming the landscape of personalized medicine by enabling tailored treatment strategies based on an individual’s genetic profile. This approach allows healthcare providers to move beyond a one-size-fits-all model and instead develop interventions that are specifically designed for each patient’s unique genetic makeup. For example, in oncology, genomic profiling of tumors can identify specific mutations that drive cancer growth, allowing oncologists to select targeted therapies that are more likely to be effective for individual patients.
Furthermore, predictive genomics can enhance drug development processes by identifying patient populations that are more likely to respond positively to specific treatments. This stratification not only improves patient outcomes but also reduces the likelihood of adverse drug reactions, which can occur when treatments are administered without considering an individual’s genetic predispositions. As pharmaceutical companies increasingly adopt genomic data in their research and development efforts, the potential for more effective and safer medications becomes a reality.
Challenges and Limitations of Predictive Genomics in Preventive Healthcare

Despite its promise, predictive genomics faces several challenges and limitations that must be addressed for its full potential to be realized in preventive healthcare. One significant challenge is the complexity of interpreting genomic data. While advancements in technology have made it easier to identify genetic variants associated with diseases, understanding the functional implications of these variants remains a daunting task.
Many variants identified through genomic studies have uncertain significance, making it difficult for healthcare providers to offer clear guidance on risk management strategies. Additionally, there is a need for comprehensive population-based studies that account for diverse genetic backgrounds and environmental factors. Much of the existing genomic research has been conducted on predominantly European populations, which may limit the applicability of findings across different ethnic groups.
To ensure equitable access to predictive genomics benefits, it is essential to include diverse populations in research efforts and develop tools that are applicable across various demographic groups.
The Integration of Predictive Genomics into Healthcare Systems
Integrating predictive genomics into existing healthcare systems presents both opportunities and challenges.
This integration can enhance decision-making processes and enable more effective management of patients at risk for certain conditions.
However, achieving seamless integration requires significant investments in infrastructure, training, and policy development. Moreover, healthcare providers must be equipped with the knowledge and skills necessary to interpret genomic data effectively. This necessitates ongoing education and training programs for clinicians to ensure they are well-versed in the implications of genomic information for patient care.
Additionally, establishing clear guidelines for when and how to utilize predictive genomics in clinical practice is essential for standardizing care and maximizing its benefits across diverse healthcare settings.
Future Directions and Opportunities in Predictive Genomics
The future of predictive genomics holds immense potential as research continues to advance our understanding of genetics and its role in health and disease. One promising direction is the integration of multi-omics approaches that combine genomic data with other biological layers such as transcriptomics, proteomics, and metabolomics. This holistic view can provide deeper insights into disease mechanisms and enhance our ability to predict health outcomes more accurately.
Furthermore, as artificial intelligence (AI) and machine learning technologies continue to evolve, they will play an increasingly important role in analyzing complex genomic datasets. These tools can help identify novel biomarkers for disease prediction and facilitate the development of personalized treatment strategies tailored to individual patients’ needs. Additionally, public engagement and education will be crucial in fostering acceptance and understanding of predictive genomics among patients and healthcare providers alike.
As we look ahead, collaboration between researchers, clinicians, policymakers, and patients will be essential for realizing the full potential of predictive genomics in preventive healthcare. By addressing ethical considerations, enhancing education and training efforts, and investing in infrastructure development, we can create a future where predictive genomics becomes an integral part of routine healthcare practice—ultimately leading to improved health outcomes for individuals across diverse populations.