Introduction to Respiratory Rate Tracking
Respiratory rate, often quantified as breaths per minute (bpm), represents the number of inspirations and expirations an individual performs within a minute. While seemingly a simple physiological parameter, its consistent monitoring has emerged as a valuable tool in both clinical and home settings for the early detection and management of various illnesses. Deviations from an individual’s baseline respiratory rate can serve as an early warning signal, akin to a subtle tremor before an earthquake, indicating underlying physiological stress or evolving pathology. This article will explore the mechanisms, applications, and challenges associated with leveraging respiratory rate tracking for this purpose.
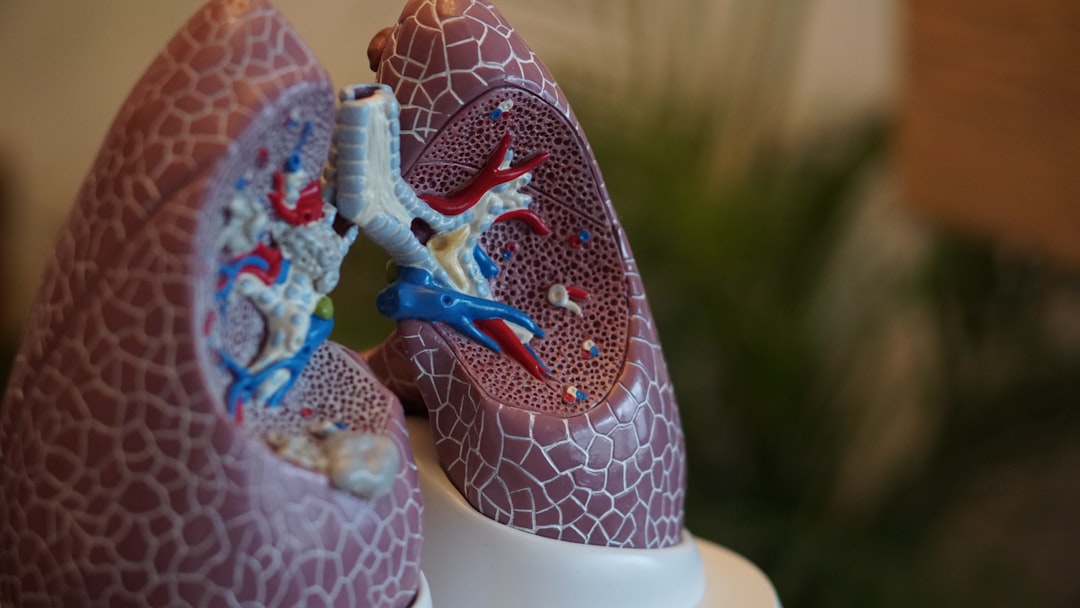
Physiological Basis and Significance
The intricate control of respiration is orchestrated by the respiratory center in the brainstem, which integrates signals from chemoreceptors, mechanoreceptors, and the cerebral cortex. This regulatory system ensures appropriate gas exchange to maintain arterial blood gas homeostasis.
Chemoreceptor Input
Chemoreceptors, located both centrally (in the brainstem) and peripherally (in the carotid bodies and aortic arch), are acutely sensitive to changes in blood pH, partial pressure of carbon dioxide (PCO2), and to a lesser extent, partial pressure of oxygen (PO2). An increase in PCO2 or a decrease in pH stimulates these receptors, leading to an increased respiratory rate to expel excess carbon dioxide, a primary acid in the body. Conversely, a significant drop in PO2 also triggers an increase in respiratory rate, though less potently than changes in PCO2.
In the realm of health technology, the importance of monitoring vital signs such as respiratory rate cannot be overstated, especially for early illness detection. A related article that explores advancements in wearable technology and its impact on health monitoring can be found at this link. This article discusses how innovative devices, including smart headphones, are being integrated with health-tracking features, potentially offering users a comprehensive approach to managing their well-being.
Mechanoreceptor Input
Mechanoreceptors, residing within the airways and lungs, respond to stretch and irritation. The Hering-Breuer reflex, for example, is activated by lung inflation, inhibiting further inspiration and promoting exhalation. While this reflex is less dominant in adults, its role in preventing overinflation is significant. Irritant receptors, sensitive to noxious stimuli, can also provoke coughing or changes in breathing patterns.
Cerebral Cortex Influence
Voluntary control over breathing, such as holding one’s breath or sighing, demonstrates the influence of the cerebral cortex. Pain, anxiety, and stress can also alter respiratory patterns, often leading to increased rates. These non-pathological influences underscore the importance of establishing individual baselines and contextualizing any deviations.
Pathological Alterations
Numerous medical conditions can directly or indirectly impact respiratory rate. For instance, fever, a common symptom of infection, elevates metabolic rate, which in turn increases CO2 production and thus respiratory rate. Sepsis, a severe systemic inflammatory response, often presents with tachypnea due to metabolic acidosis. Respiratory infections like pneumonia or bronchitis can cause shortness of breath and an increased respiratory rate as the body works harder to maintain oxygenation amidst compromised lung function. Cardiac conditions, such as heart failure, can also manifest as an elevated respiratory rate due to pulmonary congestion and reduced oxygen delivery. Even metabolic derangements like diabetic ketoacidosis lead to Kussmaul breathing (deep, labored breathing) as the body attempts to compensate for metabolic acidosis. The respiratory rate, therefore, acts as a crucial barometer for systemic physiological health.
Methods of Respiratory Rate Tracking
The evolution of technology has broadened the scope of respiratory rate monitoring from manual observation to sophisticated automated systems.
Recent advancements in technology have made it possible to monitor vital signs more effectively, and respiratory rate tracking is emerging as a crucial tool for early illness detection. This innovative approach allows for the identification of potential health issues before they become severe, ultimately improving patient outcomes. For those interested in exploring how technology is reshaping healthcare, a related article discusses the latest trends in consumer electronics, including the best Toshiba laptops of 2023, which can be found here. These devices are increasingly being used in telemedicine and health monitoring applications, highlighting the intersection of technology and healthcare.
Manual Counting
The traditional method involves observing the rise and fall of the chest or abdomen and counting the occurrences over a set period, typically 15 to 30 seconds, and then extrapolating to a full minute. While simple and cost-effective, it is susceptible to observer bias, patient awareness leading to altered breathing patterns, and is impractical for continuous monitoring, especially during sleep.
Contact-Based Sensors
These devices require direct contact with the body.
Chest Belts
Chest belts, often incorporating piezoelectric sensors or strain gauges, detect thoracic or abdominal expansion and contraction. They provide a continuous and relatively accurate stream of data, but their physical presence can be uncomfortable for prolonged use and may interfere with sleep quality for some individuals.
Electrocardiography (ECG)-Derived Respiration (EDR)
ECG electrodes, primarily designed for cardiac monitoring, can also be utilized to derive respiratory signals. The electrical impedance across the chest changes with lung inflation and deflation, and these subtle variations can be extracted from the ECG waveform. EDR offers a non-invasive approach using existing medical equipment, making it particularly useful in clinical settings where ECG monitoring is already established. However, its accuracy can be influenced by patient movement and the quality of the ECG signal.
Photoplethysmography (PPG)-Derived Respiration (PDR)
PPG, commonly found in pulse oximeters and many smart wearables, measures changes in blood volume in the microvasculature. These changes are intrinsically linked to cardiac activity, but respiratory effort also modulates the venous return and intrathoracic pressure, leading to subtle variations in the PPG waveform. Algorithms can then process these variations to estimate respiratory rate. PDR is appealing due to its widespread availability in consumer devices, but its accuracy can be challenged by motion artifacts and poor perfusion.
Non-Contact Sensors
These technologies offer the advantage of monitoring without physical attachment to the individual.
Infrared Thermography
Infrared cameras can detect temperature changes around the nostrils and mouth caused by the inflow of cooler ambient air during inspiration and the outflow of warmer exhaled air. This method is discreet and suitable for continuous monitoring, especially in sleep laboratories. However, ambient temperature fluctuations and facial obstructions can affect its accuracy.
Radar and Radio Frequency (RF) Sensors
Radar and RF sensors emit electromagnetic waves and detect the reflected signals. Respiratory movements cause minute shifts in the distance between the sensor and the body, leading to Doppler frequency shifts in the reflected wave. These shifts are then analyzed to determine respiratory rate. This technology offers excellent privacy and can penetrate light bedding, making it ideal for bedroom monitoring. It is also less susceptible to environmental interference compared to infrared methods. However, the initial cost can be higher.
Video-Based Tracking
Utilizing standard or specialized cameras, video-based tracking employs computer vision algorithms to detect subtle chest and abdominal movements. This method is entirely unobtrusive and can be implemented with existing camera infrastructure in some healthcare settings or smart homes. Challenges include susceptibility to lighting variations, occlusion, and the computational intensity required for real-time processing.
Applications in Early Illness Detection
The ability to continuously monitor respiratory rate offers a proactive approach to healthcare, moving beyond reactive responses to symptoms.
Pre-Symptomatic Illness Identification
Changes in respiratory rate often precede overt symptoms by hours or even days. For instance, a subtle but sustained increase in resting respiratory rate can be an early indicator of developing infection before fever or malaise become apparent. This “canary in the coal mine” effect allows for timely intervention, potentially preventing the progression to severe illness. Wearable devices, by collecting longitudinal data, can establish an individual’s normal baseline, making deviations more readily identifiable.
Monitoring Chronic Conditions
For individuals with chronic conditions like asthma, COPD, or congestive heart failure, respiratory rate can serve as a critical biomarker for disease exacerbations. A gradual upward trend in resting respiratory rate might signal worsening lung function or fluid overload, prompting patients and clinicians to adjust medications or seek medical attention before a crisis develops. This empowers patients to actively manage their conditions and can reduce emergency department visits.
Post-Operative Surveillance
Post-surgery, patients are at risk for complications such as pneumonia, atelectasis, and opioid-induced respiratory depression. Continuous respiratory rate monitoring can provide early alerts for these adverse events, allowing for prompt intervention. A significant drop in respiratory rate might indicate over-sedation, while an increasing rate could signal a developing respiratory infection.
Sleep Apnea Detection
During sleep, disruptions in breathing, characteristic of sleep apnea, manifest as periods of absent or reduced airflow. While definitive diagnosis often requires polysomnography, persistent changes in baseline respiratory patterns during sleep, such as repetitive apneas and hypopneas, can be detected by continuous respiratory rate tracking systems, prompting further investigation.
Challenges and Limitations
Despite its promise, respiratory rate tracking for early illness detection faces several hurdles.
Baseline Variability
Establishing an accurate individual baseline is crucial. Respiratory rate is influenced by numerous factors, including age, gender, fitness level, emotional state, body position, and recent activity. A single “normal” range is insufficient. Robust algorithms must account for these personal variations and learn an individual’s unique respiratory fingerprint over time.
Artifacts and Noise
Movement, talking, coughing, and even environmental vibrations can introduce artifacts into sensor data, making it difficult to accurately extract the true respiratory signal. Advanced signal processing techniques are often required to filter out noise and improve accuracy. For non-contact methods, factors like ambient temperature, air currents, or the presence of other individuals in the monitoring field can also interfere.
Algorithm Accuracy and Validation
The algorithms used to derive respiratory rate from raw sensor data vary in their sophistication and accuracy. Rigorous validation against gold-standard methods (e.g., capnography or pneumotachography) in diverse populations and clinical scenarios is essential. A misinterpretation by an algorithm could lead to false alarms, causing unnecessary anxiety and burden on healthcare systems, or worse, miss crucial early warning signs. The “false positive” vs. “false negative” balance is a critical design consideration.
Regulatory and Ethical Considerations
The deployment of continuous health monitoring systems raises important questions regarding data privacy, security, and informed consent. Who owns the data? How is it protected? What are the implications of sharing this sensitive health information? Regulatory bodies are still developing frameworks for these emerging technologies. Furthermore, there’s the ethical dilemma of “alarm fatigue” – an excessive number of alerts diminishing their perceived importance, and the potential for increased anxiety in individuals constantly monitoring their health metrics.
Clinical Integration and Actionability
For respiratory rate data to be truly useful, it must be seamlessly integrated into existing clinical workflows and provide actionable insights. Simply presenting raw data to clinicians or individuals is insufficient. Intelligent alert systems, clear visualizations, and decision support tools are necessary to translate raw data into meaningful clinical guidance. The challenge extends to educating both patients and healthcare providers on how to interpret and respond to these novel data streams. Implementing such systems requires careful consideration of scalability, interoperability with electronic health records, and the training of personnel.
Future Directions
The field of respiratory rate tracking is dynamic, with continuous advancements shaping its future.
Multi-Parameter Fusion
While respiratory rate is a valuable biomarker, its diagnostic power is significantly enhanced when combined with other physiological parameters such as heart rate, heart rate variability, skin temperature, sleep quality, and activity levels. Fusing data from multiple sensors creates a more comprehensive physiological profile, allowing for a more nuanced and accurate assessment of health status, much like a detective assembling various clues to solve a case. Machine learning algorithms are particularly adept at identifying complex relationships within such multi-parameter datasets, potentially uncovering subtle patterns indicative of illness that single parameters might miss.
Artificial Intelligence and Machine Learning
AI and machine learning are poised to revolutionize respiratory rate tracking. These technologies can learn individual baselines, identify subtle trends, and even predict the likelihood of illness based on deviations from these baselines. They can also help in filtering out noise and artifacts, improving data accuracy. Predictive analytics, driven by AI, could move healthcare from a reactive model to a truly proactive one, flagging potential health issues before they become critical. Consider a system that learns your unique sleep breathing pattern and can, over time, discern the early deviations that signal the onset of a respiratory infection, long before you even feel a cough.
Miniaturization and Wearable Integration
The ongoing miniaturization of sensors and the increasing sophistication of wearable technology will make continuous, unobtrusive respiratory rate tracking more accessible to the general population. Imagine smart textiles woven with sensors that monitor your breathing throughout the day and night without you even noticing. This ubiquitous monitoring will generate vast amounts of data, fueling further advancements in AI and personalized health insights. The challenge will be to ensure these consumer-grade devices maintain a sufficient level of accuracy and reliability for medical applications.
Personalized Thresholds and Alerts
Generic “normal” ranges for respiratory rate are inadequate for early illness detection. Future systems will leverage an individual’s historical data to establish personalized thresholds for alerts. An 18 bpm rate might be normal for one individual but an elevated rate for another whose typical baseline is 12 bpm. These personalized alerts will reduce false positives and increase the clinical relevance of the data, ensuring the “warning bell” rings only when truly needed. The goal is to provide highly contextualized information that empowers individuals and clinicians to make informed decisions about health.
Conclusion
Respiratory rate tracking, a seemingly simple physiological measurement, is emerging as a powerful tool for early illness detection. From manual observation to sophisticated non-contact sensors and advanced AI algorithms, the methods for monitoring respiration are evolving rapidly. While challenges related to baseline variability, data accuracy, and ethical considerations persist, the potential benefits in pre-symptomatic identification, chronic disease management, and post-operative surveillance are substantial. As technology continues to advance and our understanding of human physiology deepens, respiratory rate tracking will play an increasingly vital role in shifting healthcare towards a more proactive, personalized, and preventive paradigm, empowering individuals to take a more active role in managing their own health.
FAQs

What is respiratory rate tracking?
Respiratory rate tracking involves monitoring the number of breaths a person takes per minute. It is a vital sign that can provide important information about a person’s respiratory and overall health status.
How can respiratory rate tracking help in early illness detection?
Changes in respiratory rate can be an early indicator of illness, such as infections or respiratory conditions. By continuously monitoring respiratory rate, healthcare providers can detect abnormalities sooner, allowing for timely intervention and treatment.
What methods are used to track respiratory rate?
Respiratory rate can be tracked using various methods, including wearable devices, bedside monitors, and smartphone applications. These tools use sensors to detect breathing patterns and provide real-time data.
Who can benefit from respiratory rate tracking?
Respiratory rate tracking is beneficial for individuals with chronic respiratory diseases, elderly patients, and those at risk of infections. It is also useful in clinical settings for monitoring patients’ health status continuously.
Are there any limitations to respiratory rate tracking for illness detection?
Yes, factors such as physical activity, stress, and measurement inaccuracies can affect respiratory rate readings. Therefore, respiratory rate tracking should be used alongside other clinical assessments for accurate illness detection.