Cell therapy is a groundbreaking approach in the field of medicine that involves the administration of living cells to treat various diseases, including cancer. This innovative treatment modality harnesses the body’s own cellular mechanisms to combat illness, offering a more personalized and potentially effective alternative to traditional therapies such as chemotherapy and radiation. At its core, cell therapy aims to repair, replace, or regenerate damaged tissues or cells, thereby restoring normal function.
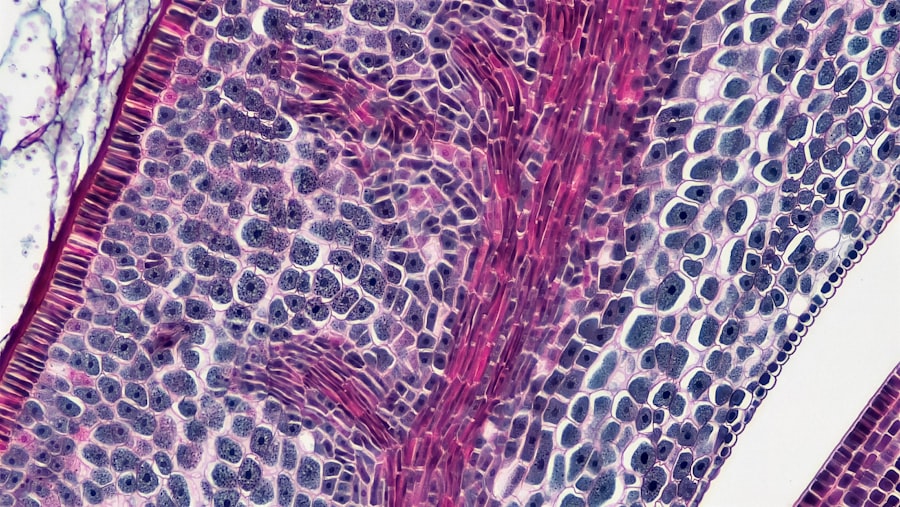
The concept has evolved significantly over the past few decades, transitioning from experimental procedures to established treatment options for certain conditions. The mechanisms by which cell therapy operates are diverse and complex. For instance, stem cells, which have the unique ability to differentiate into various cell types, can be utilized to regenerate damaged tissues.
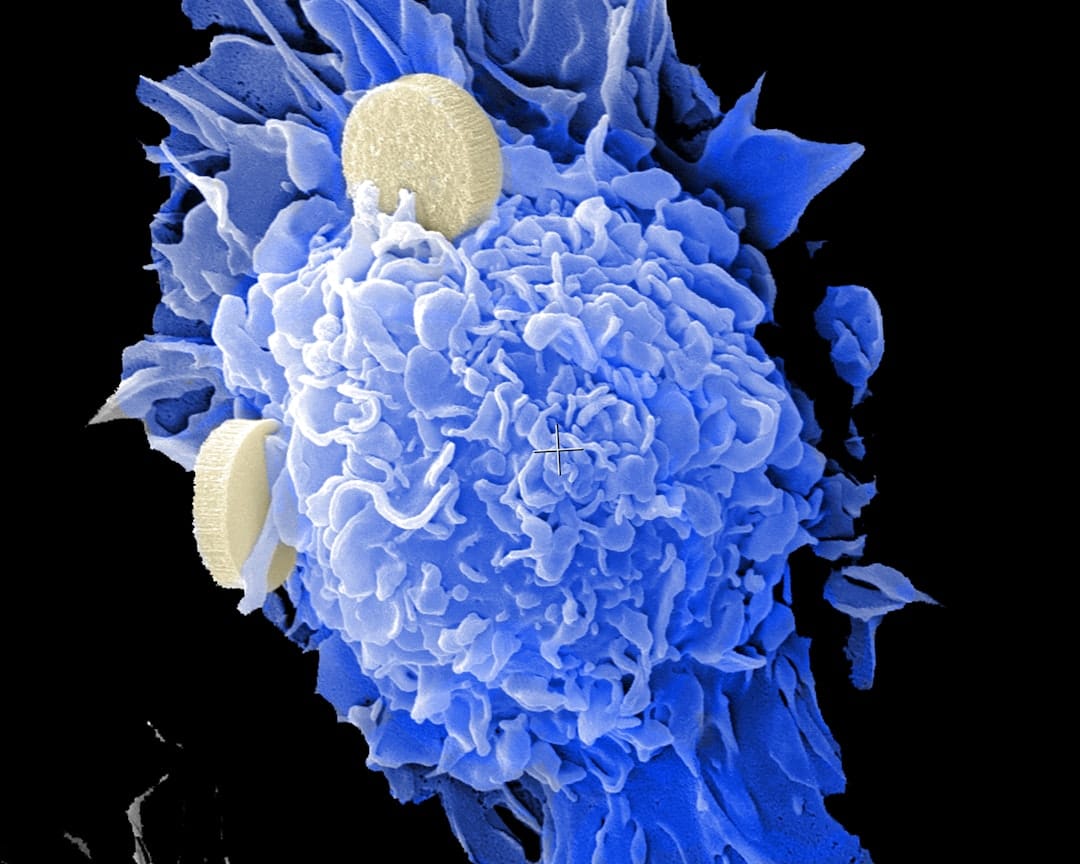
In the context of cancer, cell therapy often involves the use of immune cells, such as T cells, which are engineered to recognize and attack cancer cells more effectively. This approach not only targets the tumor directly but also enhances the body’s overall immune response against malignancies. As research continues to advance, the potential applications of cell therapy are expanding, promising new avenues for treating diseases that were once deemed incurable.
Key Takeaways
- Cell therapy involves using living cells to treat or prevent diseases, including cancer.
- Types of cell therapy for cancer include CAR-T cell therapy, TIL therapy, and stem cell transplant.
- Immunotherapy holds promise in cancer treatment by using the body’s immune system to target and destroy cancer cells.
- Challenges and limitations of cell therapy include high cost, potential side effects, and limited accessibility.
- Success stories of cell therapy for cancer include patients achieving remission and prolonged survival.
- The future of cell therapy in cancer treatment involves advancements in technology and personalized medicine.
- Access and affordability of cell therapy can be limited, posing ethical considerations in providing equal access to all patients.
- Ethical considerations in cell therapy for cancer include informed consent, patient privacy, and equitable distribution of resources.
Types of Cell Therapy for Cancer
There are several distinct types of cell therapy employed in the treatment of cancer, each with its own mechanisms and applications.
These engineered receptors enable T cells to recognize specific proteins on the surface of cancer cells, thereby enhancing their ability to target and destroy tumors.
CAR T-cell therapy has shown remarkable success in treating certain hematological malignancies, such as acute lymphoblastic leukemia (ALL) and certain types of lymphoma. Another significant type of cell therapy is stem cell transplantation, which is often used in conjunction with high-dose chemotherapy or radiation. In this procedure, hematopoietic stem cells—cells that can develop into various blood cell types—are harvested from either the patient (autologous transplant) or a donor (allogeneic transplant).
Following intensive treatment to eradicate cancerous cells, these stem cells are reintroduced into the patient’s body to restore healthy blood cell production. This approach has been particularly effective for patients with blood cancers like multiple myeloma and leukemia, providing a pathway to recovery when other treatments have failed.
The Promise of Immunotherapy
Immunotherapy represents a revolutionary shift in cancer treatment paradigms, leveraging the body’s immune system to fight cancer more effectively. Unlike traditional therapies that directly target cancer cells, immunotherapy aims to enhance or restore the immune system’s natural ability to recognize and eliminate malignant cells. This approach encompasses a variety of strategies, including monoclonal antibodies, immune checkpoint inhibitors, and cell-based therapies like CAR T-cell therapy.
The promise of immunotherapy lies in its potential for long-lasting effects and reduced side effects compared to conventional treatments. For instance, immune checkpoint inhibitors work by blocking proteins that inhibit immune responses, thereby allowing T cells to attack cancer more vigorously. This class of drugs has shown remarkable efficacy in treating melanoma and non-small cell lung cancer, leading to durable responses in some patients.
The ability of immunotherapy to generate memory immune responses also raises hopes for preventing cancer recurrence, making it a compelling area of research and clinical application.
Challenges and Limitations of Cell Therapy
Despite the significant advancements in cell therapy for cancer treatment, several challenges and limitations persist that hinder its widespread adoption and effectiveness. One major challenge is the complexity and cost associated with manufacturing personalized therapies like CAR T-cell treatments. The process involves collecting a patient’s T cells, genetically modifying them in a laboratory setting, and then reinfusing them into the patient.
This intricate procedure can take weeks and requires specialized facilities and expertise, leading to high costs that may not be covered by insurance. Moreover, not all patients respond favorably to cell therapies. Factors such as tumor heterogeneity—the presence of diverse cancer cell populations within a single tumor—can complicate treatment outcomes.
Additionally, some patients may experience severe side effects from these therapies, including cytokine release syndrome (CRS) or neurotoxicity in the case of CAR T-cell therapy. These adverse effects can limit the applicability of cell therapies to certain patient populations or necessitate additional interventions to manage complications.
Success Stories of Cell Therapy for Cancer
The landscape of cancer treatment has been significantly altered by success stories emerging from cell therapy applications. One notable example is the case of Emily Whitehead, a young girl diagnosed with acute lymphoblastic leukemia (ALL). After failing conventional treatments, she became one of the first pediatric patients to receive CAR T-cell therapy in a clinical trial.
The results were nothing short of miraculous; her leukemia went into remission, and she has remained cancer-free for years since her treatment. Emily’s story has become emblematic of the transformative potential of CAR T-cell therapy and has inspired further research into similar approaches. Another compelling success story involves patients with multiple myeloma who have undergone autologous stem cell transplantation following high-dose chemotherapy.
Many patients have experienced significant improvements in their quality of life and overall survival rates after this procedure. For instance, studies have shown that patients who receive stem cell transplants can achieve long-term remission and even complete responses to treatment. These success stories not only highlight the efficacy of cell therapies but also underscore their potential to change the trajectory of cancer care for countless individuals.
The Future of Cell Therapy in Cancer Treatment

As research continues to evolve, the future of cell therapy in cancer treatment appears promising yet complex. Ongoing studies are exploring novel approaches to enhance the efficacy and safety of existing therapies while also investigating new cellular targets for treatment. For example, researchers are examining the potential of using natural killer (NK) cells—another type of immune cell—in cancer therapy due to their ability to recognize and kill tumor cells without prior sensitization.
Additionally, advancements in gene editing technologies such as CRISPR-Cas9 hold great promise for improving cell therapies. By enabling precise modifications to genes within T cells or other immune cells, researchers can potentially enhance their anti-tumor activity or reduce unwanted side effects. The integration of artificial intelligence and machine learning into drug discovery processes may also accelerate the identification of new therapeutic targets and optimize treatment protocols tailored to individual patients.
Access and Affordability of Cell Therapy
While the advancements in cell therapy are remarkable, access and affordability remain significant barriers for many patients seeking these innovative treatments. The high costs associated with manufacturing personalized therapies often translate into substantial out-of-pocket expenses for patients or their families. For instance, CAR T-cell therapies can cost upwards of $373,000 per patient, not including additional expenses related to hospitalization or supportive care during treatment.
Moreover, disparities in healthcare access can exacerbate these challenges. Patients in rural or underserved areas may face difficulties accessing specialized centers that offer advanced cell therapies. Insurance coverage varies widely across different plans and regions, leading to inequities in who can benefit from these cutting-edge treatments.
Addressing these issues will require concerted efforts from policymakers, healthcare providers, and pharmaceutical companies to ensure that all patients have equitable access to potentially life-saving therapies.
Ethical Considerations in Cell Therapy for Cancer
The rapid development and implementation of cell therapies raise important ethical considerations that must be addressed as these treatments become more prevalent in clinical practice. One primary concern revolves around informed consent; patients must fully understand the risks and benefits associated with experimental therapies before agreeing to participate in clinical trials or receive treatment. This is particularly crucial given the complexity of procedures like CAR T-cell therapy and the potential for severe side effects.
Additionally, ethical dilemmas arise regarding the sourcing of cells used in therapies. For example, stem cells derived from embryos raise moral questions about the status of human life and the implications of using such cells for research and treatment purposes. Furthermore, as gene editing technologies become more integrated into cell therapies, concerns about unintended genetic modifications or long-term consequences on future generations must be carefully considered.
Engaging diverse stakeholders—including patients, ethicists, scientists, and policymakers—in ongoing discussions about these issues will be essential for navigating the ethical landscape surrounding cell therapy in cancer treatment.
A related article to “How Cell Therapy Is Offering New Hope for Cancer Patients” is “Discover the Best Software for Logo Design Today.” This article discusses the importance of branding and how having a well-designed logo can help businesses stand out in a crowded market. To read more about this topic, check out the article com/discover-the-best-software-for-logo-design-today/’>here.
FAQs
What is cell therapy?
Cell therapy is a type of treatment that uses living cells to help repair, replace, or improve the function of damaged tissues or organs in the body.
How does cell therapy work for cancer patients?
In the context of cancer treatment, cell therapy involves using a patient’s own immune cells, such as T cells, to target and destroy cancer cells. This can be done through techniques such as CAR-T cell therapy, where T cells are genetically modified to better recognize and attack cancer cells.
What are the potential benefits of cell therapy for cancer patients?
Cell therapy offers new hope for cancer patients by providing a targeted and personalized treatment approach. It has shown promising results in treating certain types of cancer that may not respond well to traditional treatments like chemotherapy or radiation therapy.
What are the challenges or limitations of cell therapy for cancer patients?
While cell therapy has shown great potential, there are still challenges to overcome, such as managing potential side effects and ensuring the long-term effectiveness of the treatment. Additionally, the high cost and limited availability of cell therapy can be barriers for some patients.
What are some examples of cell therapy being used in cancer treatment?
CAR-T cell therapy is one of the most well-known examples of cell therapy being used in cancer treatment. It has been approved for certain types of blood cancers, such as leukemia and lymphoma, and continues to be studied for its potential in treating other types of cancer.